Simone Einzmann writing for FOCUS GESUNDHEIT
Billions of bacteria and fungi have their habitat on our skin. Scientists are slowly recognising the significant impact these settlers have on endemic diseases such as psoriasis and atopic dermatitis
Rob Dunn has seen more belly buttons than anyone else in the world, probably more than he ever wanted to. Just as every other budding scientist, the American biologist assumed at the start of his career that his research would change the world. That he was going to spend his days digging out lint from other people’s navels or use cotton buds to scrape dirt from orifices was never a part of his vision. “Belly buttons are definitely a little weird, almost ridiculous, yet what we discovered there is anything but”, Dunn explains enthusiastically.
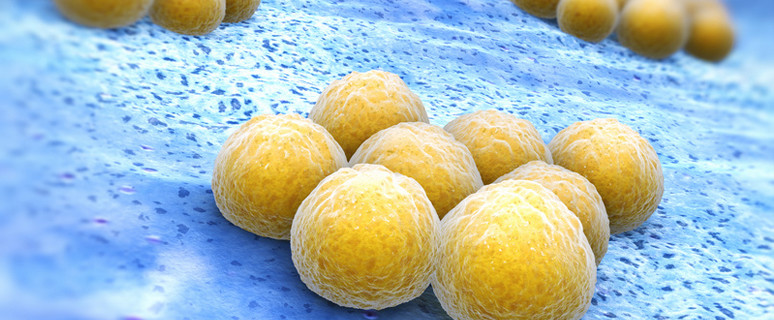
Our belly buttons are alive. This is the stunning result of Dunn’s navel expeditions. They teem with life, with bacteria, fungi, viruses. A previously unchartered territory our navels are much more than merely a hiding place for lint or an anchoring point for piercings. Rather like a microbial rain forest – with an abundance of species only waiting to be discovered. Dunn has unearthed more than a thousand previously unknown bacteria species. And he is not alone in his search. All over the globe, scientists inspect armpits or rub cotton buds between toes and buttocks. The bacterial settlers of our skin – commonly called ‘skin flora’ – have been catapulted into the focus of the scientific community. Researchers were able to show that these microbes contribute to the occurrence of atopic dermatitis, psoriasis, and acne. But at the same time bacterial communities protect the skin from pathogens and help wound healing. “As yet, we know fairly little about our tiny cohabitants, but one thing has become clear: they have a significant influence on our health”, Dunn explains.
Most people know bacteria only as germs which make us sick. Scientists, however, are confronted with a picture in which the line between good and evil is blurred. “We should avoid seeing bacteria as individual actors”, explains Jens-Michael Schröder, microbiome researcher at the University Hospital Schleswig-Holstein in Kiel. “It is only by analysing the complex interactions of microbes on our skin that we will be able to find out how they influence our skin’s health.”
At least seven billion microscopic organisms settle on our skin which has a surface area of approximately two square meters. The skin of an embryo is entirely germfree, it is only during birth that colonisation begins. Bacteria, viruses, and fungi settle on the skin, its folds, surfaces, and furrows. Which organisms establish themselves on our skin depends largely on our genetic makeup, but also on our surroundings, the climate, and even our sex. Women, for example, have a much larger variety of bacteria strains on their hands even though they wash them twice as often as men do.
We’re constantly accommodating new species in our skin’s bacterial zoo. The closer we get to someone, the more physical contact we have, the more likely we are to share his or her microbes. Members of a family will have similar skin microbiota. In much the same way, dogs and their owners or athletes on the same team will have specific microbes in common. We are always acquiring new settlers and leave our own behind: on grab poles in public transport or on ATM keyboards. Some microbes will stay, others will pay only a short visit.
For the bacterial settlers, humans are a habitat which offers a wide variety of environmental conditions: the humid armpits are from the point of view of a microbe completely different from the smooth, dry skin of our forearms or our forehead’s greasy surface. Microorganisms prefer to settle in close proximity to cutaneous glands to feed on their secretions. Near these nutrient hotspots, population densities explode to several million microbes per square centimetre, compared to a mere several hundred organisms on dry forearms. “Just as an edelweiss would immediately perish in the desert, each bacterial species has clear preferences for specific skin areas”, explains Schröder.
Out of the air, from door handles computer keyboards and polite handshakes, new bacteria arrive on our skin every day. In the competition for nutrients, autochthonous microorganisms clash with intruders. To kill the invaders, the defenders produce tiny proteins, referred to as antimicrobial peptides. We profit from our bacteria’s bulwark: by protecting themselves from intruders, they protect us. Yet these beneficial organisms are only the first line of defence. Our skin, too, has its own armoury. Specific proteins in the upper skin layer kill dangerous microbes by punching holes into them or robbing them of vital nutrients. Any harmful foreign organisms which make it through this protective barrier are received by the skin’s immune cells, called Langerhans cells, and if possible incapacitated by mobilised white blood cells.
The symbiosis of microbes and man is an evolutionary stroke of genius. Our tiny commensuals are bodyguard, cleaning service, and warning system rolled into one. Millions of years of co-evolution have resulted in a perfect collaboration between man and microcosm. Yet it remains a complex, highly unstable system. Any change may throw a spanner into this well-oiled works. Disinfectant cleaning agents, antimicrobial soaps, and similar achievements of modern civilisation are environmental disasters for our sensitive microcosm. Even though our skin will never be swept entirely clean, with bacteria surviving in skin crevices, glands, or hair follicles, the natural balance has been disturbed. An almost sterile skin presents a huge problem to skin health. Even wounds heal fastest if a wide range of bacterial species are present, as Elizabeth Grice, microbial researcher at the University of Pennsylvania, discovered. “Microbial diversity is incredibly important”, says Grice, “Infectious bacteria can also be found on healthy skin, but they are kept in check by the other bacteria.”
What happens when skin bacteria no longer do what they are supposed to is currently investigated by a number of scientists in Europe as part of the “Microbes in Allergy and Autoimmunity Related to the Skin” project (MAARS). Among them are Jens-Michael Schröder, skin researcher and biochemist at the University Hospital in Kiel, and Bernhard Homey, dermatologist at the University Hospital in Dusseldorf. The scientists look into the role bacteria play in the development of skin diseases such as atopic dermatitis and psoriasis. “We try to understand why the huge number of bacteria on our skin will usually not harm us, and why, out of the blue, a disease might break out”, Schröder says.
Microbes not only interact with each other, but also with the host’s skin. “We are convinced that microbes share information with the skin’s immune cells”, Homey explains. This is interesting in that a misprogrammed immune system plays a key role in both atopic dermatitis and psoriasis. “Now all we have to do is to identify how this communication may be manipulated”, Homey says.
The Researchers were able to map a number of ways in which bacteria influence skin diseases: They discovered that people with atopic dermatitis have fewer antibacterial agents in their skin, meaning that harmful bacteria establish themselves more rapidly: “We have found that people who suffer from atopic dermatitis have an exceedingly high concentration of staphylococcus aureus bacteria in the affected areas”, Homey explains. “These pathogens produce toxins which directly impact the immune system and trigger an inflammatory response”. Since people with atopic dermatitis also have, as a result of their genetic makeup, a more permeable skin, bacteria may penetrate more easily and deeply.
While people with atopic dermatitis show a deficit of antibacterial agents in their skin, the reverse has been found for psoriasis sufferers: “Psoriasis scales contain a strikingly large amount of endogenous antibiotics”, Schröder says. As a consequence, patients with psoriasis will even suffer less often from skin infections than healthy people would. “In our evolutionary past, people with psoriasis may have enjoyed an advantage”, Schröder assumes. “Like scale armour their skin would have offered protection from permeating bacteria, and small wounds would have healed better.”
The scientists think that a specific mix of bacteria might promote the various skin diseases. They arrived at this idea by observing that many skin diseases only occur in specific parts of the body. Psoriasis can be found predominately at the elbows and knees, atopic dermatitis in the crook of the arm and behind the knees, acne in the face and on the back. “Since we know that some bacterial species prefer to colonise specific cutaneous regions, this was an obvious conclusion”, explains microbiome researcher Schröder.
Obviously, not only microorganisms are to blame for scales and itches. “With skin diseases, we see a complex interplay between genetic predisposition, environmental factors, and skin microbiome”, says dermatologist Homey. “Up to now, the medical community has focused only on genes and the environment and almost completely ignored the huge influence of the microbiome.” Hence, there is a lot of catching up to do: Researchers estimate that it will take five to ten years before the respective pharmaceuticals have been developed.
Christine Lang is already a small step ahead. The microbiologist at the Technical University of Berlin started her own research company in 2001. Her aim: to develop cosmetics which support the natural skin flora. “We apply lotions and groom our skin, but ignore the microorganisms which live on it”, Lang laments. “We’re thoughtlessly using antibacterial soaps and disinfectant sprays, whereby completely destabilising our skin flora.” The scientist developed a lotion using components of harmless lactic acid bacteria. The product is intended to support the work of “good” bacteria. For Lang, this is only the beginning: “In the future we will very likely also work on medicinal microbial shower gels or deodorants which target the bacteria responsible for body odour or impure skin and leave the other bacteria undisturbed”, she says. To do so, we would have to know more about the microorganisms on our skin. “The bulk of all microorganisms on our skin remains undiscovered, and we have yet to find out for all species how they interact with each other”, Lang says. Her lotion will enter the market this year. Yet how will a bacterial lotion fare on the shelves, next to competing cosmetics consisting of shea butter and lotus flower extract? “We’re still working on our marketing strategy”, says an optimistic Lang.
This article was published in FOCUS GESUNDHEIT “Die Haut“ (2014). The complete issue is available for download as an E-paper: http://www.focus.de/magazin/magazin_gesundheit-spezial/die-haut-die-neuen-strategien-fuer-eine-schoene-und-gesunde-koerperhuelle_id_3858634.html
– See more at: https://www.gesunde-bakterien.de/mikrokosmos-haut/#sthash.8bbtZLoa.dpuf
Dieser Post ist auch verfügbar auf: German

 16. Jan 2015
16. Jan 2015 Popular
Popular Recent
Recent Comments
Comments